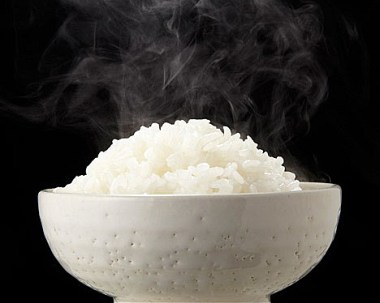
This photo accompanied the Telegraph article. While it’s beautiful, it somewhat misrepresents the research’s finding – that cooled rice contains fewer calories than hot rice. Although reheating rice after its cooled does not eliminate its resistant starch.
What happens to the starch in pasta, rice, potatoes, corn, oats, and many other starchy foods when you cook them, then allow them to cool slowly? The starch becomes resistant to our digestive enzymes. I’ve been writing about resistant starch (RS) for 10 years now so it’s probably familiar to you. Resistant starch passes through to the colon undigested and ends up feeding resident bacteria. We derive significantly fewer calories from starchy food that has been heated and cooled compared to just heated. We also derive benefit from the byproducts of the bacteria that eat the starch, e.g short-chain fatty acids and some vitamins. And, given the findings in this study, we may also derive cognitive benefit by populating our gut with beneficial RS-eating microorganisms.
Research presented at the American Chemical Society annual meeting last week described a technique for reducing calories in rice by up to 60%. You simply cook then cool the rice:
“The cooling is essential because amylose, the soluble part of the starch, leaves the granules during gelatinization,” explains [team leader Sudhair A. James]. “Cooling for 12 hours will lead to formation of hydrogen bonds between the amylose molecules outside the rice grains which also turns it into a resistant starch.” Reheating the rice for consumption, he notes, does not affect the RS levels.
Again:
RS is not broken down in the small intestine, where carbohydrates normally are metabolized into glucose and other simple sugars and absorbed into the bloodstream.
One more point. I say this often but it seems to go into the ether or something:
“After your body converts carbohydrates into glucose, any leftover fuel gets converted into a polysaccharide carbohydrate called glycogen,” [James] explains. “Your liver and muscles store glycogen for energy and quickly turn it back into glucose as needed.
People say that leftover glucose gets converted to fat. It doesn’t. It gets converted into glycogen, which is not fat.
Some headlines:
I wouldn’t call this technique “new,” would you?
New Low-Calorie Rice Could Help Cut Rising Obesity Rates, Press release from the American Chemical Society
This next title implies it’s more about the cooking. It’s not. It’s more about the cooling. By the way, this author says starch “has one central flaw: it isn’t that good for you.” The starch in potatoes, pumpkins, squashes, beans, peas, corn, carrots, barley, oats, wheat, and rice aren’t good for you. He also says that cooked potatoes are less healthful than raw potatoes. I don’t think I would ever eat a potato that wasn’t cooked:
Scientists Have Discovered A Simple Way To Cook Rice That Dramatically Cuts The Calories, Washington Post blog
Simple. Yes, it’s simple:
Simple Rice-Cooking Hack Could Reduce Calories By 60 Per Cent, The Telegraph
It’s true, eat it cold for fewer calories. But you can also reheat it if you don’t like it cold. Reheating won’t eliminate the resistant starch. In fact, the more you reheat and recool, the more resistant starch you create:
‘Eat Rice Cold For Fewer Calories’, BBC









