The cholesterol in cheese, especially aged cheese, is prone to oxidation.
It looks like dietary cholesterol contributes to the progression of various types of cancers. I first saw it here:
Cholesterol Oxides And Carcinogenesis, Journal of Clinical Laboratory Analysis, 1991
“Experimental evidence indicates a relationship between cholesterol α-epoxide and skin cancer, and exposure of skin fibroblasts to ultraviolet radiation enduces formation of significant levels of this oxide. Colon cancer is also etiologically linked to cholesterol oxidation products. Higher than normal levels of cholestanetriol have been found in patients with colon cancer and also in those with precancerous disorders such as adenomatous polyps and ulcerative colitis. Higher than normal levels of cholesterol α-epoxide have been found in breast fluid aspirates of women with benign breast disease, with or without atypical hyperplasia of the epithelium, and this may be a factor in the increased incidence of breast cancer associated with hyperplasia. Similarly, the observed increased levels of cholesterol α and β-epoxides in prostatic fluid of men with benign prostatic hypertrophy may be associated with subsequent development of prostate cancer.
Although investigations into the role of cholesterol oxidation products in cancer are still in the early stages, evidence to date indicates a potentially significant role in the induction of some types of cancer.”
These authors wrote an entire textbook on this subject:
Biological Effects of Cholesterol Oxides, 1991
“In recent years, researchers have accumulated a growing body of evidence linking cholesterol oxides with human diseases such as atherosclerosis and cancer. This book presents what is presently known about the biological activities of cholesterol oxides and is intended to stimulate thinking in new areas of diet-heart or diet-cancer research.”
So… skin cancer, colon cancer, breast cancer, and prostate cancer are all linked to dietary cholesterol … “dietary” meaning the kind we eat, not so much what our bodies make, because the cholesterol we eat is more vulnerable to oxidation – from exposure to air, heat, light, processing, radiation, and acids, e.g. stomach acids, and it is the oxidation of cholesterol which makes it more harmful. According to Dr. Clark (see link below):
“Cholesterol oxidized by the body is negligible compared to oxidized cholesterol obtained from the diet.”
Why isn’t this common knowledge? How do groups that advise eating a high-cholesterol, high-animal food diet, like Paleo and Atkins, reconcile this?
A few more…
Promotion Of Carcinogenesis And Oxidative Stress By Dietary Cholesterol In Rat Prostate, Carcinogenesis, 2004
Researchers gave mice a diet supplemented with 1% cholesterol. For relativity’s sake, in humans, 1% of a 2000-calorie diet is 20 calories or about 2 grams of cholesterol. That’s about 6 or 7 times the recommended limit of 300 mg/day. So, these mice were getting a lot of cholesterol.
- Rats on the high cholesterol diet developed adenocarcinoma in the ventral prostate more frequently (26% versus 4%).
- Rats on the high cholesterol diet demonstrated a higher incidence of atypical prostatic hyperplasia (24% versus 4%).
- These results indicated that long-term feeding of a 1% cholesterol diet promoted carcinogenesis and tissue oxidative stress in rat prostate.
Promotion Of Colon Carcinogenesis Through Increasing Lipid Peroxidation Induced In Rats By A High Cholesterol Diet, Cancer Letters, February 1996
Here, rats that were exposed to a carcinogen and then fed a high-cholesterol diet developed colon cancer at a significantly higher rate than those not fed a high-cholesterol diet. The authors speculated that “cholesterol may potentiate the carcinogenicity of [a carcinogen] in rats via an increase of lipid peroxidation and decrease in the activity of peroxidase in the target organ.”
Effect Of Dietary Oxidized Cholesterol On Azoxymethane-induced Colonic Preneoplasia In Mice, Cancer Letters, October 1992
Here, rats were getting just 0.1% cholesterol (about 220 mg on a 2000-calorie diet). And “a dose-response relationship was observed in both mouse strains between the level of dietary cholesterol or oxidized cholesterol and formation of preneoplastic aberrant crypt foci. These anomalies were enhanced to a greater extent by oxidized cholesterol. This data shows a very strong effect of cholesterol in enhancing the development of preneoplastic lesions in chemically induced cells.
And finally… as I was searching for studies that addressed dietary cholesterol and cancer, I ran across this review article:
The Cholesterol Story: Are Your Fighting Heart Disease? John Clark, M.D, 2009
Clark says the same as the studies above, referencing them too:
“A high cholesterol diet depresses natural killer cells activity by 75%, making cholesterol a dangerous food if you want your immune system to fight off viruses responsible for pandemic flu, cancer or autoimmune diseases. In fact, oxidized cholesterol increases the risk of skin cancer, colon cancer, ulcerative colitis leading to cancer, breast disease leading to cancer, and prostate hyperplasia leading to cancer.”
It’s just 8 pages, almost 3 of which contain over 300 references. He backs his claims meticulously. Nonetheless, it’s quite readable. He accompanied it with some videos. I have to say, his lecture is one of the most accessible I’ve come across on this topic. Comprehensive, explanatory, and refreshingly lacking in the ego you see in lectures at universities and teaching hospitals … where, it seems, the number of acronyms filling a sentence is proportionate to the intelligence and credibility of the deliverer, or so the deliverer thinks. (Note: Clark’s site is religiously affiliated.)
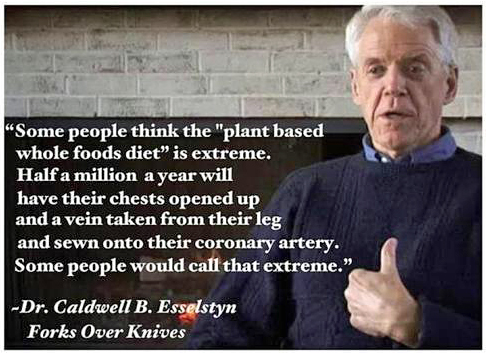
Clark concludes with a nod to a low-fat, whole food, plant based diet, a diet that eliminates all oxidized cholesterol. (Only animal food contains cholesterol, and that cholesterol, owing to its treatment before consumption, is oxidized to some degree.)